Why sampling perilymph with intratympanic drug application tells you almost nothing about the drug's properties
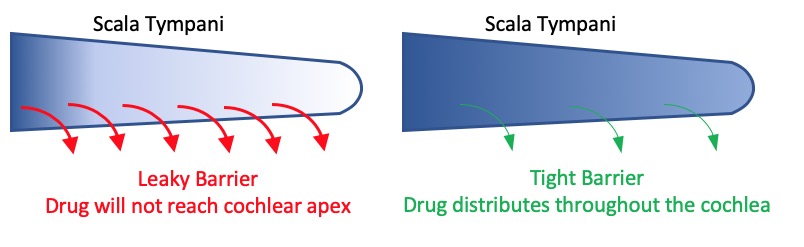
How drugs spread along the ear depends highly on how easily the molecule is lost to the vasculature. As drugs spread predominantly by diffusion, if the drug is lost quickly to the vasculature (such as dexamethasone) it will never reach the apical regions of the cochlea, as shown in the left panel of the figure below. Instead, a steady-state will be established with a sustained drug gradient along the ear. If the drug is lost more slowly, it will then be able to diffuse throughout the cochlea, as shown at the right side of the figure. Knowing the rate of drug leakage from perilymph (known as the rate of elimination or clearance) is critical to understanding how far the drug will distribute along the ear.
When drugs are applied intratympanically, they have to pass through the round window membrane to reach perilymph. The rate-limiting barriers for drug passage through the round window and the vascular epithelium are both cellular layers with tight junctions. Specifically, the middle ear epithelium covering the round window and the vascular endothelial cells making up the capillaries of the vasculature. A problem arises because drugs that easily pass through one boundary (the round window) will also easily pass through the second boundary (vascular walls)(See our page on "Drug Properties” and egg plots). Small lipophilic molecules (such as dexamethasone) pass easily through membranous boundaries while large, hydrophilic polar molecules (such as gentamicin) pass less readily.
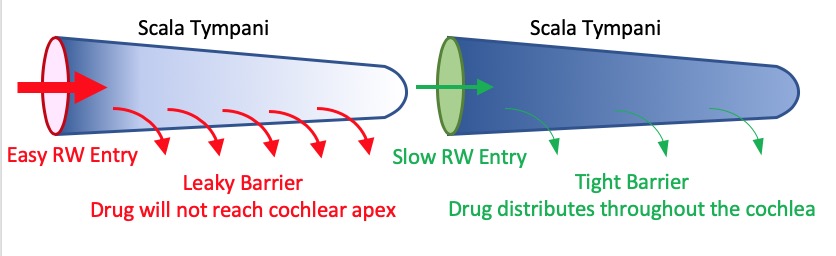
An interesting consequence of this dependence is that a similar perilymph drug concentration and time course can occur at the base of the cochlea for a drug with fast entry and fast elimination and for one with slow entry and slow elimination.
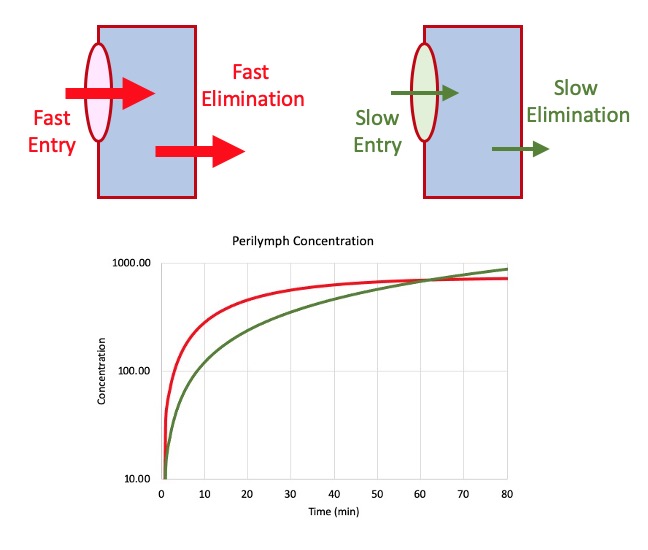
In this example, time courses were calculated for entry and exit into a simple one-compartment model. Half times used in the calculations were 600 min and 15 min for “fast” entry and elimination respectively and 1500 and 300 min respectively for “slow” entry and elimination respectively. It can be seen that measuring the perilymph concentration at the base of the cochlea will not allow you to differentiate between these two conditions. The method of "sequential sampling", which measures drug gradients along the length of scala tympani, can be used to verify how the drug spreads.
What this means:
It means that “Taking and analyzing a perilymph sample from the basal part of the cochlea tells you almost nothing about the pharmacokinetics of the drug in the ear”.
Also note that the calculation above assumes a constant, sustained drug level in the middle ear. In most cases, drug concentration declines rapidly in the middle ear which adds a declining time course to the concentration generated, making sample concentrations at the base of the cochlea even more difficult to interpret.
Maybe it isn't a problem: If it means that whatever the kinetics, some drug will enter and be present in the basal part of the ear. If you are treating the basal part of the ear, then this may be totally fine. Basal turn concentration may be somewhat independent of kinetic properties.
There is a solution to the PK problems this creates:
It is possible to measure the rate that a drug is eliminated from perilymph by injecting drug solution directly into perilymph. When done correctly, the entire inner ear can be loaded with drug. Perilymph can then be sampled at various time points afterwards so that the concentration decline with time can be measured. This allows a reliable elimination rate to be established.
The above perspective is based on experimental data and became apparent in a study comparing the kinetics of triamcinolone and triamcinolone-acetonide (Salt AN, Hartsock JJ, Piu F, Hou J. Comparison of the pharmacokinetic properties of triamcinolone and dexamethasone for local therapy of the inner ear. Frontiers in Cellular Neuroscience 2019; 13, 347. https://www.frontiersin.org/article/10.3389/fncel.2019.00347). In that study, triamcinolone and triamcinolone-acetonide were found to have completely different kinetics, yet measured perilymph concentrations of the two drugs in the basal part of the ear were very similar.
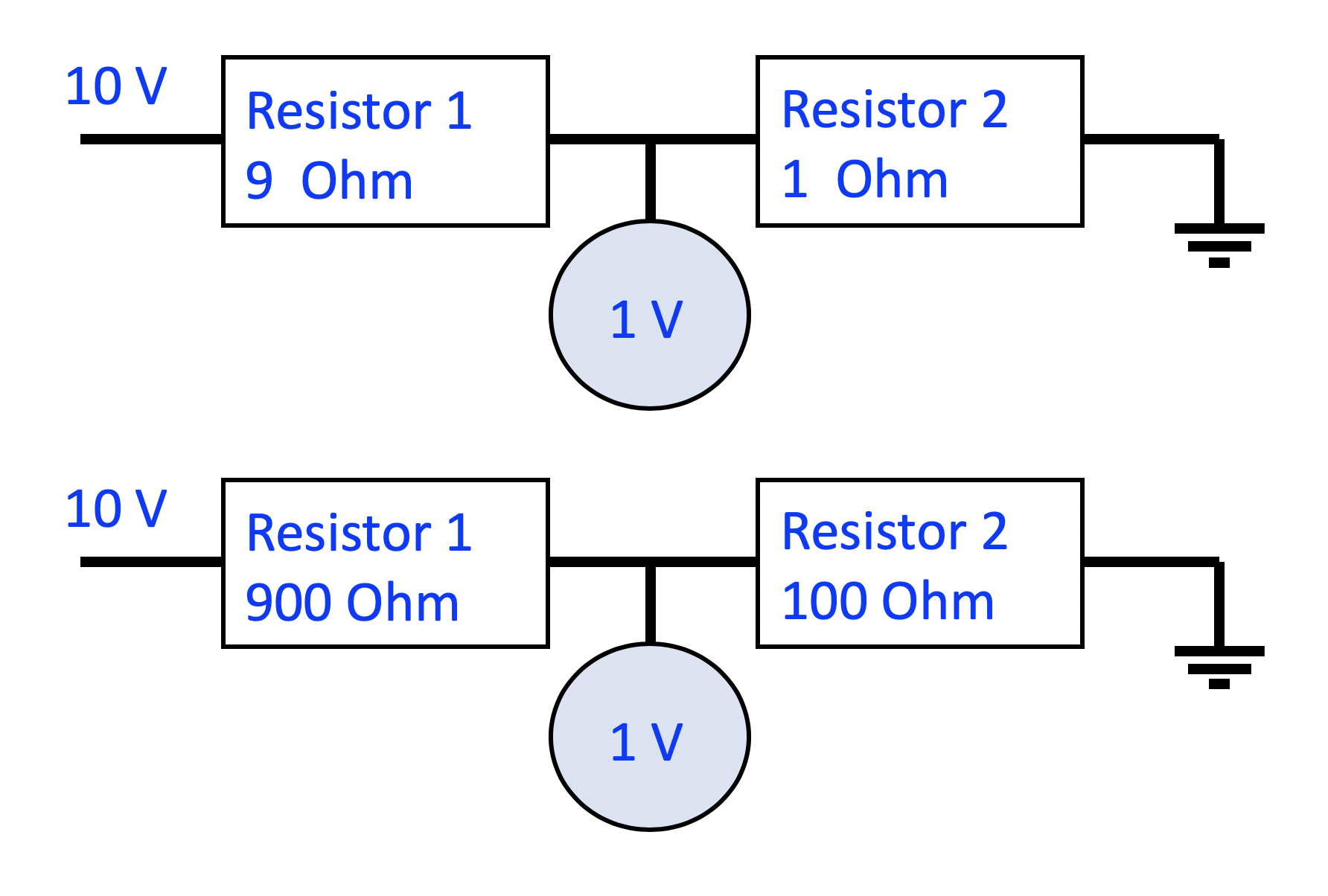
Having two barriers in series is comparable to the simple resistor network shown below. The voltage measured between the two resistors (analogous to perilymph concentration) gives a measure of the ratio of the two resistors, but not their absolute values. A measurement of 1V would occur with resistor pairs of 1 Ohm: 9 Ohms; 100 Ohms: 900 Ohms or 1 mOhm: 9 mOhms. You cannot derive the magnitude of the resistors from the measurement.
Be aware that interpreting drug concentrations in samples taken from the basal part of an animal's ear, and inferring how that drug may distribute in the human ear, is extremely difficult. In most cases, additional, more detailed PK studies are required.
